A new combination therapy found for acute leukaemia

Researchers at Tampere University recently published a study that demonstrated the efficacy of a new combined therapy for childhood leukaemia. The study is a part of a larger research project focusing on personalised cancer treatments.
Leukaemia has several subtypes. Acute leukaemia is most often diagnosed in young children, but sometimes also in adults. The study at hand concentrated on the most frequent type of cancer in children, the B-cell acute lymphoblastic leukaemia (B-ALL). About 3-5% of patients with this diagnosis have the TCF3-PBX1 fusion gene expression that promotes disease development.
Chemotherapy is usually effective in this type of cancer, but the cancer easily reoccurs. In addition, the cancer may become resistant to chemo drugs, which further exacerbates the prognosis.
“In principle, our group is not so much studying leukaemia as such, but certain molecules whose levels are high in the bodies of cancer patients,” says Daniela Ungureanu, Academy of Finland Senior Research Fellow and leader of the Cancer Signalling research group at Tampere University.
Combination therapy clearly improved the efficacy of medicines
Previous studies have found that the levels of two proteins are elevated in this subtype of leukaemia. One of these proteins acts as a receptor on the surface layer of cancer cells and is called ROR1 (receptor orphan-like receptor) and the other is a ligand (Wnt16) that binds itself on the surface of abnormal cells. Elevated levels of these molecules point to the fact that these proteins play an important role in the survival of cancer cells.
Medical therapies are usually more effective if there are more of their target compounds in cancer cells. The side effects of chemo drugs are usually smaller the less their target compounds are found in the healthy cells of the body.
When the function of these proteins was inhibited, medical treatments worked much better. A combination therapy, where the function of the receptor was disabled and the cancer cells exposed to specific cancer medicine, turned out to be especially effective.
“We showed that these proteins act together in this type of leukaemia. Inhibiting the function of the receptor improved the efficacy of certain medicines, such as venetoclax and navitoclax especially,” Ungureanu explains.
Personalised therapies are the future of cancer research
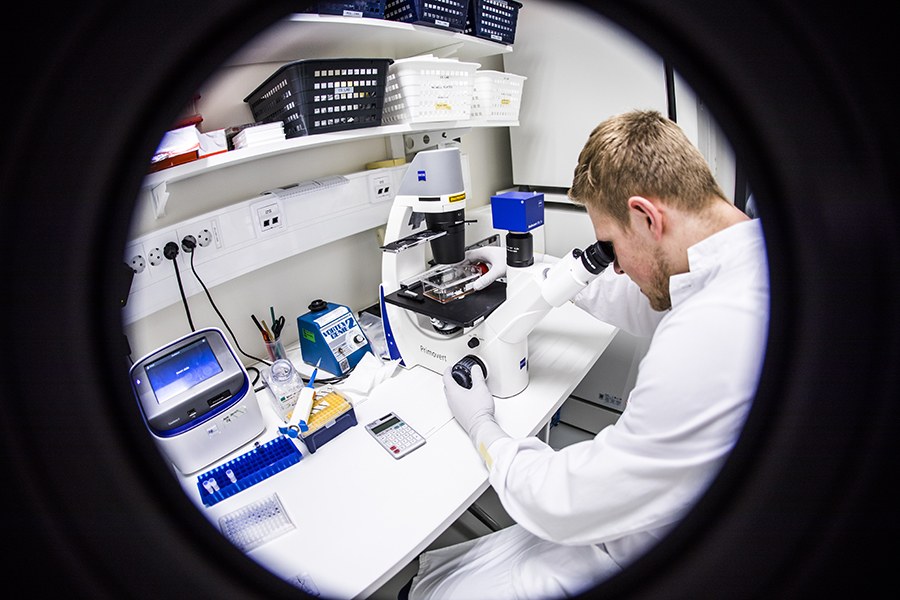
Finding medicines that are more effective entails systematic work where different possibilities are tested one by one. When cancer is diagnosed, a blood and bone marrow sample is taken from the patient. In the laboratory, cancer cells are isolated from the samples and grown in incubators ex vivo. The new cancer cells are exposed to many different drugs in order to find the best possible treatment for the patient.
In the study conducted at Tampere University, the cancer cells were exposed to 660 different oncology drugs.
“Even though two people suffer from the same cancer, same medicines do not necessarily work. Cancer mutates quickly. It also rapidly develops resistance to medical treatments,” Ungureanu says.
That the cancer cells are not completely similar inside the body and in laboratory conditions brings another challenge into the picture.
“We are only starting this work. However, personalised medicine is a much better operating model compared to testing each drug on patients by trials and errors. In cancer treatment, it is important to find the right medicine as soon as possible,” Ungureanu notes.
The researchers at Tampere University are closely cooperating with the Institute for Molecular Medicine Finland (FIMM) at Helsinki University. FIMM is an international research institute that examines the mechanism of diseases on the molecular level.
“The DSRT platform (drug sensitivity and resistance testing) we used in our study was developed at FIMM. They have a wide library of oncology drugs used in the treatment of cancer. Our cooperation with FIMM is vital,” Ungureanu says.
Precision medicine decreases side effects and improves the prognosis
Traditional cancer medicines have many undesired side effects. Cancer cells multiply fast; thus, cancer medicines are developed to kill precisely the rapidly spreading cells.
However, traditional cancer medicines cannot distinguish cancer cells from healthy cells. That is why cancer treatments often cause hair loss and skin problems. Skin cells are the types of cells in the human body that multiply the fastest.
“Our study aims at developing enhanced personalised treatments. We are getting better at targeting cancer cells, which means that healthy cells suffer less from the treatment,” Ungureanu says.
Leukaemias are a set of blood cancers that are associated with an increased number of immature lymphocytes in the blood, bone marrow and lymph nodes. Leukaemias are divided into acute and chronic leukaemias, of which the acute ones kill the patient fast if untreated. They are predominantly childhood cancers. Chronic leukaemias only develop at an advanced age and proceed slowly.
Text: Jaakko Kinnunen
Pictures: Jonne Renvall





