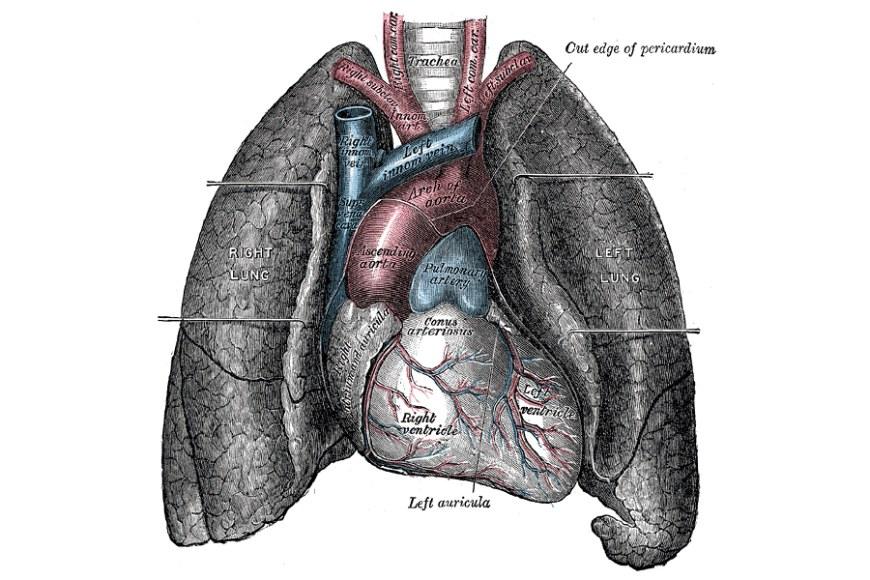
How lungs sense oxygen – a route to future therapies for acute lung failure
A paper just published in the journal Science Advances provides some tantalizing clues as to how the muscle cells surrounding the blood vessels in the lung actually detect acute oxygen deprivation and respond appropriately. The work was conducted largely by Dr Natascha Sommer from the Justus Liebig University in Giessen, Germany, within an international consortium led from Tampere University by Dr Marten Szibor and from Giessen by Professor Norbert Weissmann, and including other labs in Sweden and Germany.
The crucial cellular component where this low-oxygen signal is detected and actioned has been revealed as the mitochondria, which consume the vast majority of the oxygen used in all cells to maintain energy supply, by burning carbohydrates and fats.
Dr Szibor, based in Professor Howy Jacobs' lab in Tampere University, and who recently relocated to Jena (Germany), has been at the forefront of developing a tool to probe mitochondrial involvement in physiology and disease, based on expressing the alternative oxidase, AOX, a by-pass enzyme for the final steps of mitochondrial oxidation. AOX is absent from humans and other mammals, but is found in lower organisms such as plants, fungi and many marine invertebrates, from where the AOX gene can be sourced. Together, the research consortium showed that the vasoconstrictive response to acute oxygen deprivation in the lung is abolished when the AOX by-pass is present. This acute sensing mechanism is clearly distinct from the well-established chronic hypoxia response, for which the 2019 Nobel Prize in Medicine was awarded.
By uncovering this basic physiological mechanism, therapies can potentially be developed in the long-term, based on AOX or other mitochondrial effectors, to improve the body's oxygen supply in the event of acute lung failure. The work also underlines the fact that successful cutting-edge research with real-world applications requires intensive international cooperation between scientists and out-of-the-box thinking.
"Above all", commented Howy Jacobs, "the work further expands our understanding of the role of mitochondria in keeping cells healthy: not only as the hub of metabolism, but also where different kinds of signals are integrated to influence cell behaviour, and where medicine can intervene to correct faulty or inappropriate responses".
Sommer N, Pak O, Alebrahimdehkordi N, Pak O, Knoepp F, Strielkov I, Scheibe S, Dufour E, Andjelković A, Sydykov A, Saraji A, Petrovic A, Quanz K, Hecker M, Kumar M, Wahl J, Kraut S, Seeger W, Schermuly R, Ghofrani HA, Ramser K, Braun T, Jacobs HT, Weissmann N, Szibor M (2019) Bypassing mitochondrial complex III using alternative oxidase inhibits acute pulmonary oxygen sensing. Sci. Adv. 6, eaba0694. http://doi.org/10.1126/sciadv.aba0694
Further information:
Marten Szibor, marten.szibor [at] tuni.fi
Howy Jacobs, howard.jacobs [at] tuni.fi
Picture: Gray's Anatomy / Wikimedia Commons